Keep The Joint You Were Born With
Explore Advanced Minimally Invasive
Surgical Options for Joint Preservation
Explore Advanced Minimally Invasive Surgical Options for Joint Preservation
Benefits of Joint
Preservation vs. Total
Joint Replacement
Benefits of Joint Preservation vs. Total Joint Replacement
Joint preservation is a great option for many people who don’t qualify for total joint replacement. OSI offers surgeons new devices that can improve the way many bone and joint surgeries are performed.
A joint replacement is performed to restore form and function.
An IA Saucerization is performed to restore the biology of the bone before its form and function are lost.
Preserved Motion and
Native Anatomy of the Joint
Less Painful Recovery
Quicker Recovery Time
Can Be Performed on
Patients of All Ages and Sizes
Our devices and procedures provide a safe and effective way to preserve the joint you were born with.
We help you help patients keep the joint they were born with.

OSI Has Been Helping
Surgeons Perform Successful
Surgeries for Over 20 Years
OSI Has Been Helping Surgeons Perform Successful Surgeries for Over 20 Years
What Doctors Are Saying
Patient Stories
Frequently Asked Questions
An IA Saucerization of the knee is an advanced arthroscopy procedure that removes bone spurs and excess fat from the knee to eliminate pain and abnormal function of the knee joint while walking. A collection of bone and bone marrow, not a simple bone marrow aspiration, collected through a stab incision at the hip is converted into a bone graft slurry and then injected into the bone at the site of the excess fat, thus restoring the bone's health. The procedure also smooths over the cartilage and repairs the menisci and ensures their proper function. The surgeon must use unique entry portals into the knee; thus, the procedure requires the use of specialized arthroscopes and products designed by Orthopedic Sciences. The patient can go home on the day of surgery, and no incision is larger than 3mm. See our Patient Stories and note that our products have been used for over 20 years.
The more popularly known knee arthroscopy for osteoarthritis with a meniscus tear does not thoroughly clean and reshape the knee bones to as near normal as possible, nor does the procedure aim to ensure proper meniscus function. Currently available arthroscopic equipment is NOT designed to achieve this objective. Further, orthopaedic surgeons performing arthroscopy for osteoarthritis with a meniscus tear do not do so with an understanding of how fat under pressure within the bone causes the osteophytes to form. See Figures 9A and 9B on our Knee FAQs page. Explore our web pages and carefully read through the information presented. Search the internet for information on saturated and trans fats and how they affect the health of your bones, watch our patient testimonials, be engaged with your healthcare, share our website (www.orthopedicsciences.com) with your doctor to ask the pertinent questions, and join our efforts to help you keep the joint you were born with.
The procedure also recontours the cartilage where it is torn and ensures proper function of the meniscus during walking by cleaning or repairing the meniscus and removing any osteophytes that block the meniscus from gliding backward and forward while walking. The function of the meniscus is assessed while in surgery, and it is never assumed that the primary problem with the meniscus is the tear observed on a preoperative MRI.
Osteophytes form when excess fat attempts to escape the bone. These osteophytes are easily seen on x-ray and have a characteristic shape resulting from knee motion. During an IA Saucerization, the surgeon also decompresses the thigh bone by releasing this excess fat from the bone using percutaneous intraosseous irrigation. Cancellous bone and bone marrow are taken from the hip above the knee and then injected into the bone to replace the excess fat. The cancellous bone and bone marrow injected into the bone improve the bone’s health and strength. An IA Saucerization should not be performed using traditional arthroscopes.1 Traditional arthroscopes lack the properties of OSI’s Q Arthroscopes designed to save joints. The skilled surgeon performs the IA Saucerization through two to three small incisions while repeatedly motioning the knee as if the patient were walking. Fluoroscopy should be used during surgery as well. On the morning of surgery, the patient is asked to mark the most painful areas of the knee. This helps the surgeon focus immediately on the most painful parts of the knee during surgery. The blood pressure and heart rate are monitored for abrupt changes indicating that the areas being cleaned/reshaped contribute to the pain experienced by the patient. These painful areas are matched to the ink markings placed on the skin by the patient. The surgeon correlates the arthroscopic findings with the patient’s history, physical examination, x-rays, and MRI and ensures that the anatomy of the knee is restored to as near normal as possible and that the menisci are moving backward and forward smoothly after their cleaning or repair. The surgery can be performed with or without a tourniquet.
Additionally, OSI’s specialized bone grafting system for joint preservation allows the surgeon to collect autologous cancellous bone and bone marrow through a two to three mm incision at the hip. Your doctor may require you to use crutches for two to four weeks after surgery, and home exercises may be equally as effective as outpatient physical therapy. A continuous passive motion machine (CPM) or any other apparatus is usually not required. Given the very small incisions, significant scarring after surgery is unlikely. Most patients can go home the day of surgery.
The following steps comprise an IA Saucerization of the knee:
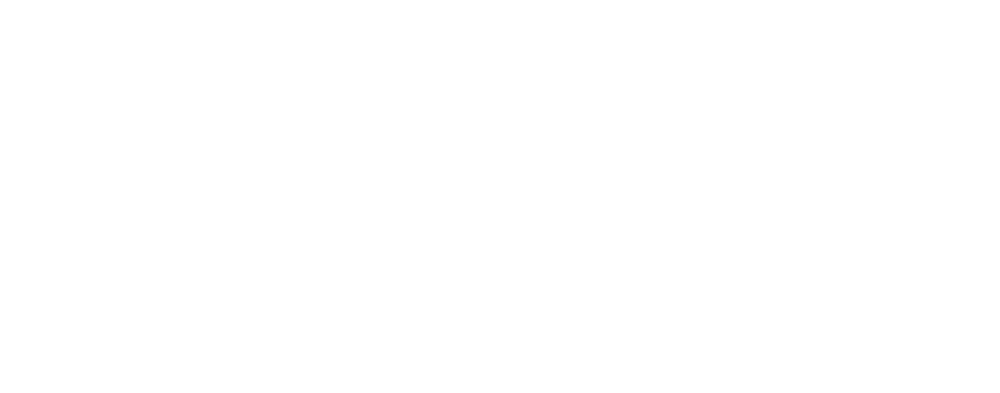
An IA Saucerization cleans and reshapes the inside of the knee and restores the biology to the bone. Basic arthroscopy for osteoarthritis is often performed as a procedure to correct mechanical problems in the knee that cause pain and locking of the knee. The underlying problems within the knee are not addressed, namely, the excess intraosseous fat and oxLDL. Additionally, the procedure is NOT performed to prevent a total knee, but rather to delay the total knee. The IA Saucerization is performed with the view that the excess fat and oxLDL must be released, the menisci must be repaired or debrided, the contours of the bone must be returned to near normal as possible, and bone graft and bone marrow must be injected into the bone where the excess fat and oxLDL have been removed. The IA Saucerization of the knee views the knee joint as the end-organ of the femur, as Fremont Chandler considered the femoral head as an end-organ, albeit related to its blood supply. Using OSI’s system, all of the harvested cancellous bone and bone marrow can be percutaneously injected into the knee bones after it has been irrigated, and there is no waste. See our patient testimonials. After this reading, we are certain that others will begin to recommend or promote their bone marrow concentrating products for injecting bone marrow concentrate into the bone after arthroscopy. But here again, the oxLDL and excess fat should be removed along with the removal of all osteophytes to the extent possible. The indications to perform an IA Saucerization of the knee for osteoarthritis may be the same as those for performing basic arthroscopy of the knee for osteoarthritis with a meniscus tear. Basic arthroscopy for osteoarthritis with a meniscus tear addresses the torn meniscus and may also include a degree of debridement of other structures. Even if the surgeon intends to perform extensive debridement of the knee and does so, traditional arthroscopic equipment and techniques, having been developed in the 1970s, do not fully allow this to be accomplished. Peer-reviewed publications on such debridement do not describe the quality of the debridement performed but conclude that debridement is not effective.1,2 Additionally, when performing basic arthroscopy, no efforts are made to address the health of the bone or the process that led to the formation of the offending osteophytes. In the case of an IA Saucerization of the knee, the surgeon inserts the arthroscope at the top of the knee beneath the patella through OSI’s patented Clear Cannula. The inside front, sides, and back of the knee can be observed. The OSI Clear Cannula elevates the patella to improve visibility without damaging it. See Figures 1 and 2.
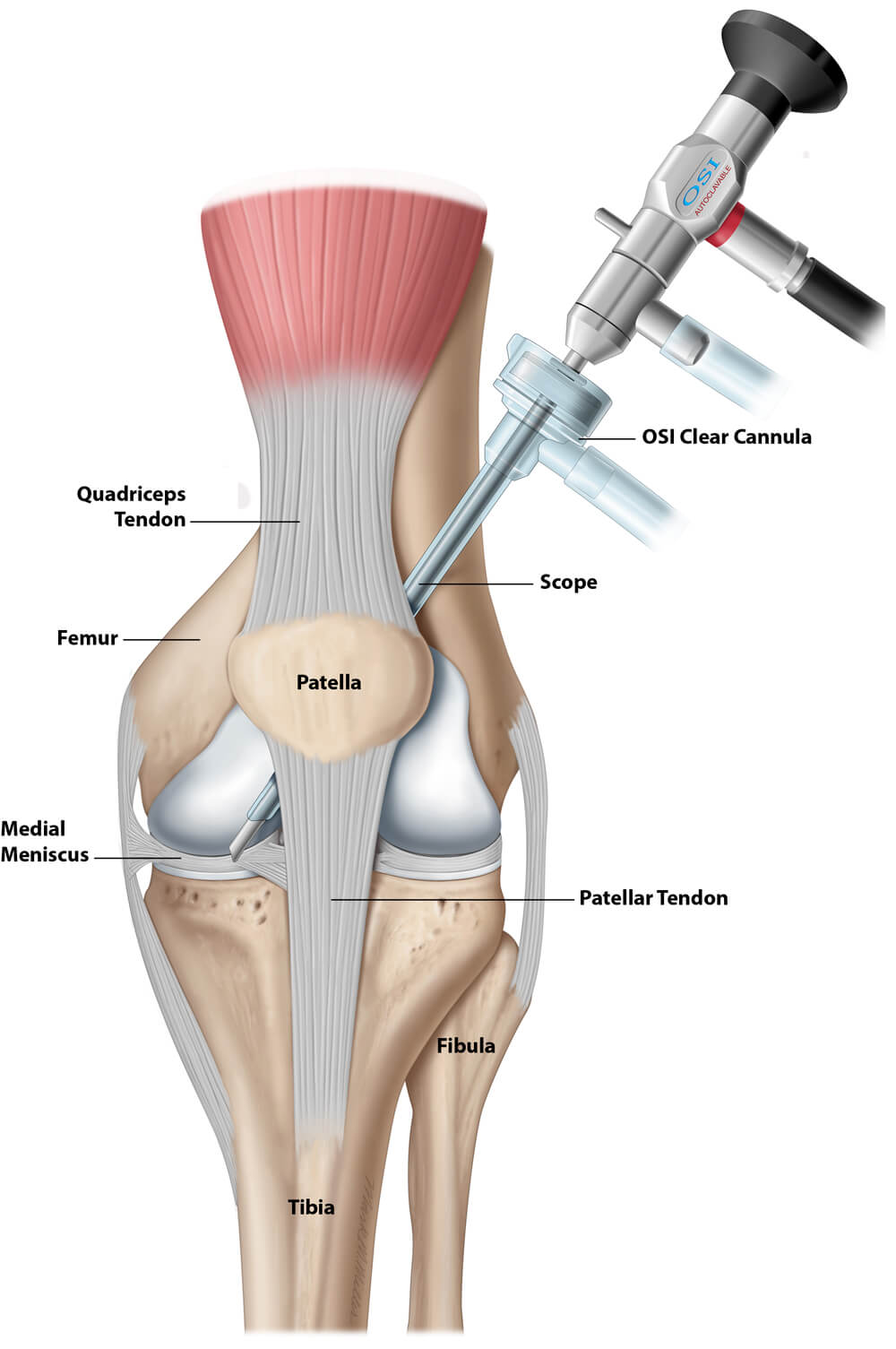
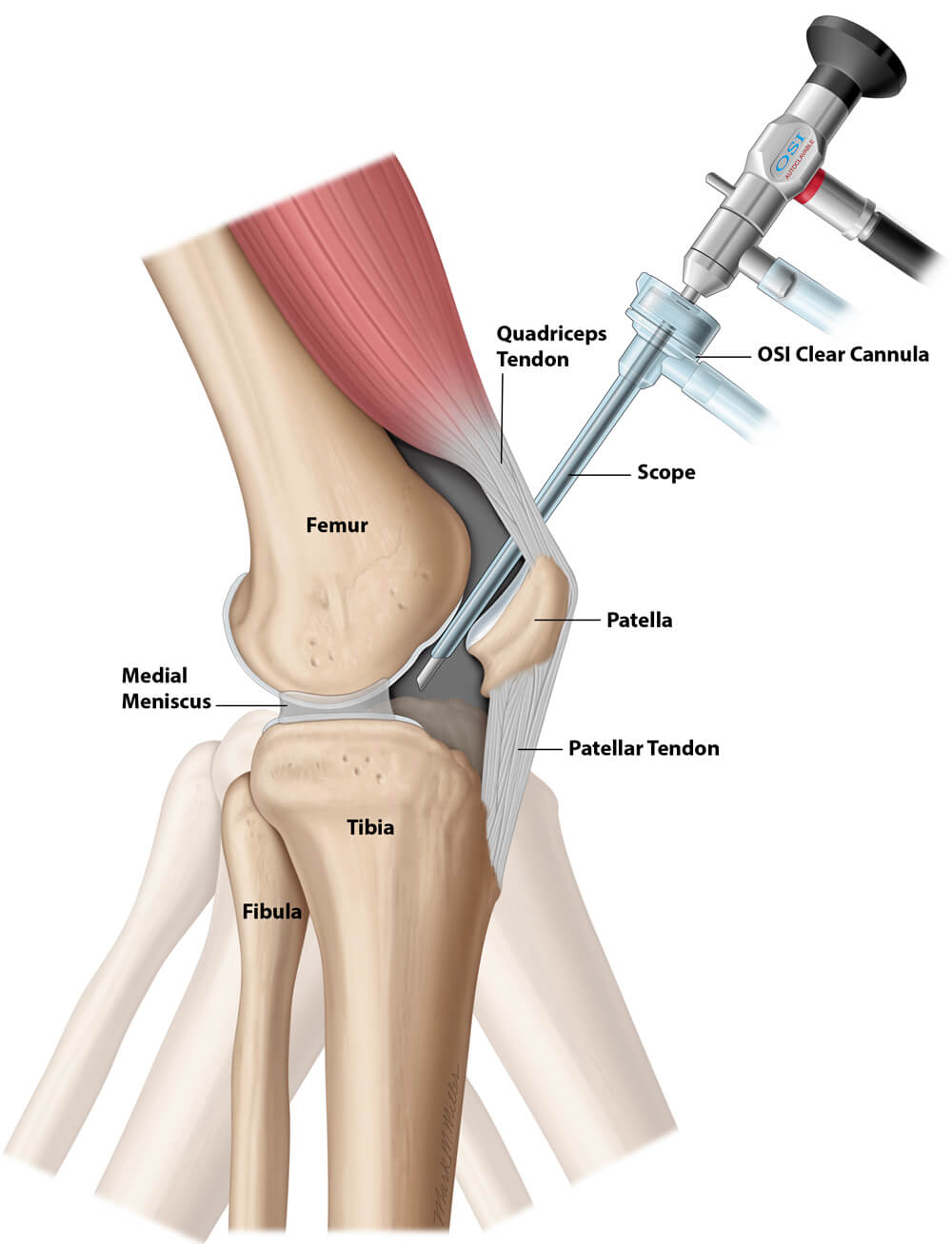
The Q Arthroscope and Clear Cannula allow the surgeon’s assistant to motion the knee during surgery as if the patient were walking or stooping. This motion aids in locating the areas that make the knee snap, lock, or pop and cause pain. In contrast, a traditional arthroscope is inserted below the patella in the front of the knee. The surgeon cannot see behind the tip of the arthroscope (blind spots) nor how the tibia and menisci move along the femur while walking because the arthroscope must move as the doctor moves the tibia. See Figure 3.
Inserting a traditional arthroscope at the top of the knee may damage the cartilage because these arthroscopes are too short and too large. Even if inserted safely, a traditional arthroscope does not provide the surgeon with the non-digital 3D images required for a successful IA saucerization, as does OSI’s Q Arthroscopy system with Clear Cannula. For many years, the deficiencies of traditional arthroscopes have not been recognized because most arthroscopists consider themselves excellent technicians when performing arthroscopy, and the goal of surgery is frequently to “repair or clean the torn meniscus,” with meniscus tears being considered a sports injury or a “degenerative” tear. As a result, arthroscopy for osteoarthritis with a meniscus tear is commonly performed with much ongoing debate about its effectiveness. The IA Saucerization requires using OSI’s patented arthroscopic equipment and cannulas to create a non-digital 3D view of the inside of the knee joint. OSI developed its arthroscopy system to improve the debridement of the knee joint, not to resolve the debate of the effectiveness of arthroscopy among professionals. Patented specialized burrs and shavers allow access to the back of the knee to reshape the bones and cartilage so the meniscus can glide along the cartilage as it should. See our Safety PX video under Cartilage Surface Products. Standard arthroscopy equipment does NOT allow the surgeon to complete an IA saucerization of the knee successfully and should not be attempted. Doing so will lead to exacerbation of the pain experienced by the patient.
Experts differ on whether knee arthroscopy is a worthwhile treatment option for knee osteoarthritis. Many experts comment on clinical studies suggesting knee arthroscopy does NOT benefit patients with knee osteoarthritis.1,2 Some surgeons argue that because knee arthroscopy is less invasive, it is worth trying before moving forward with a more invasive irreversible total knee replacement. It is important to note that the clinical studies that reported no benefit from arthroscopy do NOT describe decompressing the fat within the bone. These clinical studies used traditional equipment and techniques that included lavage (washing the knee out with saline) and removing osteophytes that were immediately visible or free-floating inside of the joint. Many other structures may have been debrided as well. However, these clinical studies make a large assumption about the quality of the surgery performed and remain silent on how osteophytes form and how they may block the motion of the menisci. These studies do NOT comment on how the inaccessibility of various osteophytes represents a limitation of the equipment or the surgeon's skill. Further, these clinical studies do not discuss how the meniscus function may have or may not have improved after its repair or the debridement of any meniscus-blocking osteophytes. More importantly, no mention of how intraosseous (within the bone) fat may cause pain, pressure, or weakening of the bone in any stage of disease. The IA Saucerization reshapes the bones and removes nearly all osteophytes to the extent possible, releases the excess fat that blocks the inflow of blood, improves the quality of the bone with an injection of autologous cancellous bone and bone marrow into the femur and tibia, and restores the function of the meniscus. Well-known knee injections for osteoarthritis call for the chosen medicament to be injected into the joint, assuming the cartilage or its age-related degeneration (senescence) is the sole and primary cause of disease.