My Knee: Questions to Ask a Doctor

Please review our Terms of Use before proceeding. OSI wishes to repeat and make clear that by reviewing the following, either on a digital screen or in printed format, you (or any reviewer hereof) acknowledge, without exception, that you (or any reviewer hereof) have reviewed OSI’s Terms of Use and that you (or any reviewer hereof) are NOT using or intending to use the information below to seek or obtain medical advice of any kind whatsoever. The information below is simply information, and it may be presented as a question, in some cases, because health information is vast and often includes unfamiliar medical terms. Joint preservation cannot be described in one or two structured sentences or simple bullet points. A broader understanding of osteoarthritis is required for a committed surgeon to perform a successful Intraarticular Saucerization. Quick and simple answers have been avoided. The human joint is an extraordinary structure, and its preservation requires understanding its complexity.
- What does joint preservation mean in your practice?
- If a reconstruction doctor specializes in joint replacement, that’s working on the bone, and a sports doctor works on the cartilage, menisci, ligaments, and tendons, how do either of you as an individual surgeon save my joint if a good joint needs healthy bone and healthy cartilage, ligaments, and tendons?
- In talking about osteoarthritis, not a 20-year-old athlete, aren’t joint injections that use steroids, PRP, stem cells, and viscosupplements, without cleaning the joint first, just like using a mouthwash without first brushing the teeth? I have heard that some people just have an in-office injection. Should my joint be cleaned out before an injection? Would making an effort to clean my joint before an injection be helpful? If not, why not?
- I know these injections can help with pain, but if you get rid of my pain with a series of injections, is my knee actually getting better, or is my condition worsening? Is my cartilage still grinding down, leading to “bone on bone,” but I just can’t feel any pain? How is that beneficial to me if I want to save my joint? So, am I just having less pain leading up to a total knee? What if I do not want a knee replacement at all?
- Does it make sense to clean my joint thoroughly and release all the excess fat inside of the bone (not a simple lavage with the removal of maybe one or two bone spurs)? Why is a lot of fat released from the femur during a total knee, yet no one talks about how maybe all of the fat released contributes to why a total knee is a good procedure? Is there any information I can read that says the fat in the bone does not contribute to disease, nor does its release contribute to a good outcome if I were to have my knee replaced? Or have you ever even thought about this possible association? See this link https://www.youtube.com/watch?v=3TzNfpatwN0 at 4:38 - 4:40 and notice the fat released from the femur as the drill bit is inserted into the femur. This fat may contain oxLDL (bad cholesterol) that enters the joint through bone spurs and then damages the cartilage. Also, carefully listen to the surgeon describing the bone spurs at 5:27. The bone spurs result from the fat attempting to escape the femur.
- If I undergo arthroscopy for a meniscus tear, how is my knee thoroughly cleaned? Does thoroughness mean that since you are an excellent surgeon, the knee was “thoroughly” cleaned?
- Why do some say that cleaning the knee for osteoarthritis does NOT work when bone spurs may only be randomly removed, and all of the fat in the bone that is causing the bone spurs is not even released nor even considered relevant?1,2
- Some doctors that replace knees say that arthroscopy for osteoarthritis is not effective.1,2 My question is, how is arthroscopy for osteoarthritis ever to be effective if specialized equipment for thoroughly cleaning the knee is not used, and the surgeon may be thinking, “if this doesn’t work, the knee can be replaced after nine months?”3 It seems to me that many people may be relying on an article that says arthroscopy does not work, yet the article appears to describe only a small amount of cleaning, and the releasing of fat from the bone is not even mentioned.1,2
- I would like a “one and done” procedure if I am going to have my knee replaced. Since I am fairly young, will I need a revision at some point, meaning I am still not finished? Would you suggest I just forget about saving my knee because a knee replacement is one of the most successful procedures ever developed? I am not saying an Intraarticular Saucerization is a substitute for a knee replacement. The information on the OSI website specifically says it is NOT. I am only asking about a lasting solution for my knee pain during the run-up to a replacement.
- During a knee replacement, a long rod may be inserted into the thigh bone. This causes a lot of fat to be released from the thigh bone. Why would it be okay to release all of that fat during a knee replacement, yet no one has considered releasing at least some of that fat during arthroscopy? Too much fat anywhere in the body is bad, but no one considers having too much fat in the bone. Please explain this. Would you consider that maybe the excess fat inside my bone contributes to my pain and the development of osteophytes somehow? Too much fat in the blood may cause heart disease, so why would too much fat in the bone be okay or not worth considering? I know that the bone stores fat, but so do other parts of the body until the person is overweight, and that is not okay. Could a person have too much fat in their bones because of their diet?
- What does thoroughly cleaning the knee mean in your practice? Do you remove osteophytes to ensure the meniscus is not trapped in the back of the knee? Do you move my knee around during surgery as if I were walking to see where things might be contacting each other in an abnormal way? If not, why not? Do you use the proper equipment to clean my knee thoroughly, or do you use routine arthroscopes and consider the knee thoroughly cleaned because you are good at “scoping a knee?”
- If you are a knee replacement doctor, can I also expect you to be just as skilled in performing arthroscopy procedures?
- Have you ever performed an IA Saucerization of the knee? This is extensive cleaning of the joint, removing nearly all bone spurs, smoothing over the cartilage, and releasing the pressure and excess fat from the bone. The procedure also cleans or repairs the meniscus if it is damaged and infuses the knee bones with bone and bone marrow taken from my hip. I understand this bone and bone marrow to be injected into bone marrow edema lesions that are common in people with osteoarthritis. This is not an office injection into the joint of spun down bone marrow or PRP. It seems to me that many “joint” injections assume the bone has no role in osteoarthritis.
- Can you perform an Intraarticular Saucerization (IAS) on my knee if I am a candidate for the procedure? Can you perform an IAS on my knee using the specialized equipment developed by Orthopedic Sciences for this specific procedure? If you can, can I be assured that you will use the proper equipment for the specific procedure? This equipment has been available for 20 years and I have seen some great patient testimonials. If you have great outcomes, don’t you want others to know about your success? If not, why not? If you do NOT perform IAS procedures, can you learn more about the procedure, or can you refer me to someone that is interested in the procedure or learning more about it?
- What things do you consider when deciding to save a joint? How is replacing half of the joint “saving” it? I want to keep my entire joint.
- If my legs are badly bowed, maybe the only option is a total knee because you have to straighten my legs. My legs look pretty straight to me. Are straight legs easier to save than those that are crooked?
- I’m puzzled. I know that all osteophytes are removed if I have a total knee replacement; however, if I have arthroscopy for a meniscus tear associated with osteoarthritis and osteophytes, many of the osteophytes are NOT removed.1,2 Why is this the case? It seems to me some are quick to say arthroscopy does not work and then a discussion will start about how a peer-reviewed paper demonstrated that arthroscopy does not work. However, just reading the reference myself seems to show that the fat I am asking you about was not released, standard equipment was used, and the point of the paper was NOT to demonstrate any sort of good outcome but rather to document the opposite. Therefore, I have limited options, and many surgeons say arthroscopy does not work.
- How do you address the quality of my bone during arthroscopy for osteoarthritis with a meniscus tear? What about the quality of my bone if I were to have my knee replaced? I guess you are concerned about the quality of my bone when my knee is replaced, but what about the quality of my bone during arthroscopy?
- If you do not know anything about a saucerization of the knee, are you able to read about it and let me know if it can benefit me? I noticed on this web page under the Physician section there are at least 22 citations that seem to reference fat and osteoarthritis. Please explain why removing the bone spurs from my knee joint and cleaning my bone thoroughly is not a good option for me. If I were to have my knee replaced, wouldn't you remove the bone spurs from my knee? Please share with me why continued injections, physical therapy, bracing, oral medication, and more office visits are my best options until I meet what is required for my knee to be replaced.4 It seems to me that things inside my knee are just getting worse, and I have never heard of any of these options, I guess, as you say, non-invasive or non-operative procedures, preventing a knee replacement.
- I’m puzzled, what is wrong with me keeping my knee joint by trying to find a lasting solution that is helpful to me during the time that my knee can be saved? Can you refer me to someone that will at least read about this procedure, and talk to me about how the fat in my bone may be causing arthritis in my knee?
- I saw this YouTube video where this doctor says he performs 500 replacements per year. I saw a lot of fat come out of the bone during the video. Can we discuss how fat in the bone may be contributing to the progression of osteoarthritis? Again, I am not asking about being overweight. I am asking about the fat inside of the bone that seemingly is forced out of the bone making bone spurs.
- Please explain how my diet may contribute to osteoarthritis in my knee. Please don’t just say it’s my weight. Everybody that has osteoarthritis is not overweight. Please don’t just say nobody knows. I am not a doctor, but this webpage has a lot of articles that seem to explain how the fat I am asking you about could lead to osteoarthritis.
- If I had a lot of fat in my bone before a knee replacement and the fat is released, what prevents that fat from building up again, given that no one seems to think that this excess fat is relevant? Will a return of the fat and pressure within the bone make the prosthesis loose or contribute to malalignment? Will I need a revision if the prosthesis becomes loose or is malaligned? What do you say to someone that still has pain after the knee is replaced, yet it is not crooked and it is NOT infected, and you do not consider the reaccumulation of intraosseous fat around the prosthesis relevant? Do you just refer someone like this to a pain management doctor?
- If my diagnosis is osteoarthritis, are there more problems in my knee than possibly just a meniscus tear and torn cartilage? If so, are these other problems addressed if I am a candidate for arthroscopy for osteoarthritis with a meniscus tear?
- If my diagnosis is osteoarthritis with a meniscus tear and you perform arthroscopy the traditional way and only clean or repair the meniscus, how am I to expect a good outcome when there are more problems in my knee since my major problem is osteoarthritis? What about the quality of my bones? What about the excess fat, if any?
- Yes, everybody knows that a total knee is a good procedure, but can you perform an excellent arthroscopy procedure by extensively cleaning my joint? Robots are used to replace the knee, but the arthroscopy equipment used to clean the knee was developed in the 1970s. It seems to me that if and when arthroscopy is performed for osteoarthritis with a meniscus tear, the knee may not be extensively cleaned at all because the proper equipment is not used, and the doctor may be simply thinking that the knee can be replaced in nine months if the procedure fails.3
- If you are performing several joint replacements per year, how often are you trying to preserve the joint?
- Is it a good idea for me to perform home exercises after an IA Saucerization, or do I need to go to physical therapy like people who have had a total knee?
- If I am a candidate for knee arthroscopy, will all of the osteophytes be removed, followed by smoothing over the cartilage? Will the meniscus be repaired or cleaned? Will excess fat be released from the bone, and will healthy cancellous bone and bone marrow be injected into my bone? I am not talking about injecting something into my joint. I am asking about injecting bone and bone marrow into my bone, not just a spin-down of a bone marrow aspirate. If the health of my bone is good or is good enough for a replacement, why do I have osteoarthritis? Isn’t osteoarthritis a disease of the cartilage and the bone? If you say osteoarthritis is a disease of the cartilage, are you assuming that the bone is NOT diseased, or it only becomes diseased because the cartilage is bad?
- I understand that bone marrow can be taken from my hip and concentrated and then injected into my joint, but does taking bone and bone marrow from my hip and infusing it into the bad areas of my bones represent a good option to improve the health of my knee? Will you use the proper equipment to clean my knee thoroughly? It seems surprising that a doctor will use a robot to replace the knee, but when performing an arthroscopy, he or she may use an arthroscope developed in the 70s and then say arthroscopy for osteoarthritis does NOT work. I guess if the knee is poorly cleaned during arthroscopy, a good outcome should not be expected.
- Why would thoroughly cleaning my knee, as I have mentioned, be unreasonable if I am a candidate for arthroscopy?
- How are my interests in saving my joint and reading about various treatment options (e.g., Orthopedic Sciences' new website has a lot of good references) any different from reading about a knee replacement and then asking you a variety of questions about what I can expect before or after a knee replacement? Maybe my knee is so worn out that my only option is a knee replacement. If not, can we discuss thoroughly cleaning my knee using the proper equipment and restoring my bone health, if I am a candidate for joint preservation?
- Besides exercising and losing weight, what other things can I do to assist you with helping me keep the joint I was born with? I am sure that if I were scheduled to have my knee replaced, any doctor would want me to be engaged and ask these same questions.
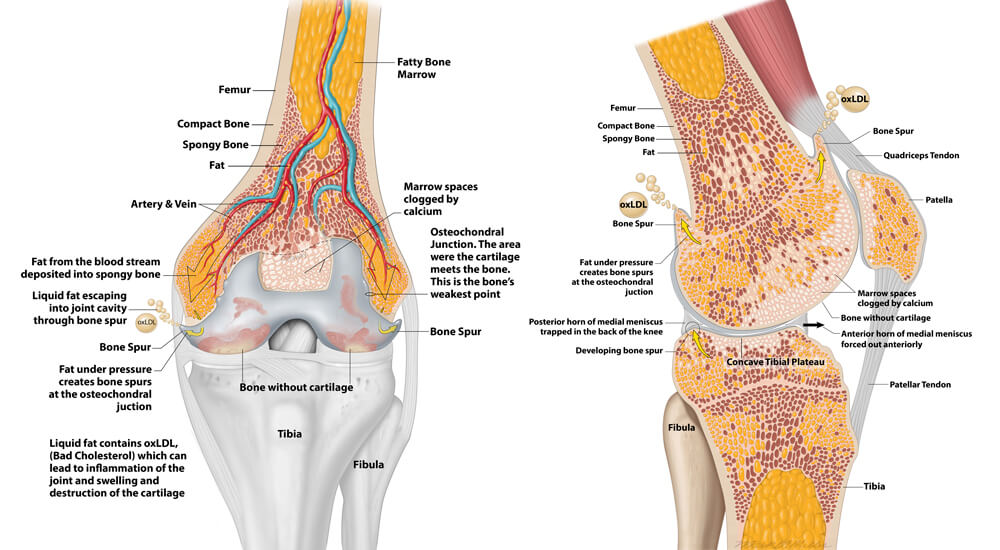
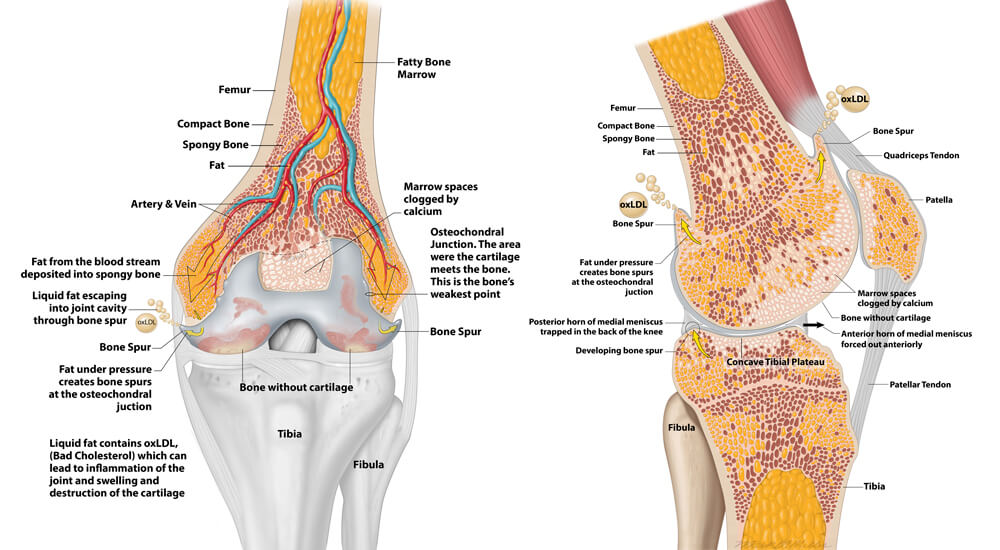
Figures 1A Left and 1B Right: Figure 1a shows the typical location of bone spurs at the osteochondral junction, OCJ. Fat is normally deposited within the bone, as it is a significant energy source for blood cell formation. However, excess fat in the diet may cause an over-accumulation of fat. The heart continues to try and deliver blood to the bone cells leading to increased pressure within the bone. The marrow spaces calcify (see above), which limits the space available for the fat. Thus, the excess fat must be displaced or consumed for blood to flow freely into the bone. The increased pressure within the bone forces the fat to exit at the OCJ, creating a bone spur upon exiting. The level of oxygen in the bone is low where the fat accumulates and leads to the oxidation of the fat and the formation of oxidized low-density lipoproteins–oxLDL. As the bone spurs develop, the oxLDL is released into the joint through the developing bone spurs causing destruction of the cartilage and inflammation of the joint, 1b. Also note how the meniscus may become trapped in the back of the knee. This is easily seen on an MRI. Therefore, if the meniscus is NOT freed up during classic arthroscopy for osteoarthritis with a meniscus tear or “mechanical symptoms,” a good outcome is less likely.
Further, simply “washing the joint out” will NOT solve this problem, as oxLDL is released into the joint continually. The above may partially explain the unfavorable results of Moseley and Kirkley. Moseley and Kirkley did not consider oxLDL and intraosseous fat accumulation in their studies. Washing the knee out and removing a few bone spurs may provide short-term relief. However, a saucerization aims to remove all bone spurs to the extent possible, allowing the release of a substantial amount of intraosseous fat. The bone is then infused with autologous cancellous bone and bone marrow where bone marrow edema lesions have developed. The infusion of the bone and bone marrow further causes the fat to exit the bone. This restores the biology of the bone. The knee is like an osteobiologic cul de sac. Accumulated fat and oxLDL must be removed to return the biology to the bone. It is important to understand the role fat plays in OA at the chemical level to preserve the joint.
Interestingly, if the knee joint were replaced, oxLDL may reaccumulate and lead to early loosening of the prosthesis because oxLDL inhibits osteoclast development. Diet and losing weight are necessary to take stress off the knee and to modify the amount of fat and oxLDL circulating in the bloodstream because oxLDL negatively affects bone formation. For 20 years, OSI developed products with this understanding, and many patients over an extensive age group have avoided a joint replacement using our technology. See our
Patient Stories.
Important Information
Intraarticular Saucerization of the Knee
An Intraarticular (IA) Saucerization is advanced arthroscopy of the knee and is intended for individuals with joint disease resulting from degenerative and post-traumatic arthritis, and the treating doctor has determined that the patient is a candidate for the procedure. Ask your doctor if you are a candidate for an IA Saucerization. Because your doctor cannot perform an IA Saucerization or is not familiar with an IA Saucerization does not mean you are not a candidate for the procedure. Ask your doctor if he or she can perform an IA Saucerization and if he or she can ensure the proper equipment is available for the procedure. Ask your doctor if he or she is willing to read the peer-reviewed papers about a saucerization before deciding whether you will benefit from the procedure. An IA Saucerization is not appropriate for all patients. An IA Saucerization is NOT a substitute for a knee replacement. If a given knee has met the clinical indications for its replacement, it cannot be saved with an IA Saucerization. Only a competent orthopaedic surgeon can determine if a knee can no longer be saved. An IA Saucerization is considered useful during the run-up to a knee replacement. An IA Saucerization requires significant patient involvement. You must help your doctor understand the source and location of your pain, and a modification of your diet, if it includes high amounts of saturated fats and trans fats, may be required.
In comparison, a knee replacement removes the entire knee joint, and the physician rarely, if at all, discusses the content of your diet relative to the longevity of the knee replacement. A knee replacement is not a resurfacing procedure, meaning only the surface of the bone is removed. This information is NOT provided to say a knee replacement is NOT a good procedure. A knee replacement is a well-proven, safe and effective procedure for osteoarthritis. The information we provide is to help interested parties to understand why their knee may be arthritic and how the accumulation of fat and oxLDL contribute to disease. The IA saucerization recognizes this association and has been used to save 100s of joints for 20 years. The saucerization removes the diseased painful parts of the knee and reshapes the inside of the joint, replacing the intraosseous fat with bone and bone marrow during a time in the disease process when thoroughly cleaning the knee joint can save the joint. This extensive cleaning requires special equipment. Taking chronic pain medication for months or years on end does not stop the progression of osteoarthritis. Meet with your doctor to discuss your pain and ask questions about how your diet contributes to your disease. Being advised that weight alone contributes to your knee pain is not enough and does not explain how and why someone that is of normal weight develops osteoarthritis. Further, losing weight is difficult, but providing patients with a pain-relieving procedure and discussing how diet contributes to the development of osteoarthritis may put many people in more control of their knee joint’s destiny. The engaged patient must go beyond listening to comments on the BMI, such as “you need to lose about X number of pounds, and then your knee can be replaced.” Yes, losing weight is helpful and an obese patient should lose weight. But losing weight and NOT discussing how fat is stored in the bone and how it contributes to osteoarthritis of the knee misses an opportunity to offer meaningful treatment beyond numerous knee injections, PT, pain medication, activity modification, and multiple physician office visits during the run-up to a knee replacement. We must recognize the association between fat intake and osteoarthritis beyond the stress placed on our joints due to weight. The IA Saucerization relieves the pressure in the knee, removing osteophytes and allowing the excess fat in the bone to escape. The patient must be engaged with their doctor by asking questions and recognizing that a good outcome is more than just a procedure performed well.
An IA Saucerization is the thorough cleaning of the joint. It is NOT an experiment to thoroughly clean your joint. Routine arthroscopy is a cleaning of the joint, but it is NOT as thorough as it could be because the equipment used is outdated. Also, in the past, no consideration was ever given to how excess fat in the bone contributes to disease. Your bones normally store fat. We have learned that bone spurs in the knee develop when excess fat is forced out of the bone. When these bone spurs are seen on x-ray, the patient is told they have osteoarthritis. The specialized equipment patented and developed at OSI allows a treating surgeon to thoroughly clean the knee joint, remove these bone spurs, and release the accumulated excess fat from the thigh bone. The accumulated excess fat is released as the bone spurs are removed, and an autologous cancellous bone and bone marrow slurry are injected into the areas of the bone where the excess fat and oxLDL have accumulated. OSI’s equipment further allows the congruency of the joint to be restored, enabling the menisci to slide forward and backward during walking. A surgeon ensuring that your knee joint functions normally when performing arthroscopy is not an experiment. When a trained surgeon performs the above and accesses the knee joint as described on these web pages, the procedure is called an IA Saucerization. Anyone claiming they can achieve the above with existing arthroscopic technology or that an IA Saucerization is experimental has likely misunderstood the published literature. Such comments are contradictory to Moseley and Kirkley. Moseley and Kirkley have already shown that arthroscopy using existing technology is ineffective for knee osteoarthritis. Again, a treating surgeon must be willing to read the references cited below and those under the Physician tab; and the patient must be willing to modify their diet.
Osteoarthritis of the Knee and the Role of Intraosseous (within the bone) Fat
Patients who are NOT overweight and exercise daily still develop osteoarthritis. That said, the complete cause of osteoarthritis is not known. However, excess fat leads to increased pressure within the bone, which may be further increased by hypertension and the development of osteophytes that may irritate the joint lining. These osteophytes that cause abnormal joint motion and trapping of the menisci are frequently found during arthroscopy and knee replacements in patients of ideal body weight and patients who are overweight.
An easy way to understand osteoarthritis and its relationship to fat intake is to consider coronary artery disease. In coronary artery disease, elevated levels of low-density lipoproteins (LDL) that contain triglycerides and cholesterol gain access to the internal lining of an artery. Once the LDL (Bad Cholesterol) enters the internal lining of the artery, it does not easily leave. The internal lining calcifies through a complex biologic process that includes LDL oxidation. This calcification hardens and narrows the artery and may lead to a heart attack by obstructing the blood flow to the heart muscles.
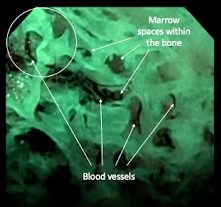
Similarly, LDL enters the bone marrow and is stored in fat cells. This fat, in excess, may obstruct the inflow of blood into the ends of the bones and through a complex process, lead to calcification of the marrow spaces through oxidation of the LDL (oxLDL).5,6 Note that in the arteries of the heart, the LDL crosses the artery wall and leads to calcification of the artery. In the bone, the LDL crosses the wall of the small blood vessels and enters the bone marrow. This LDL is oxidized and leads to calcification of the marrow spaces. Calcification of the marrow spaces makes the bone brittle. That said, it is easy to think of the insides of the bone at the knee to have the appearance of a honeycomb. Blood vessels travel through these combs and communicate with each other through a capillary network.7 In osteoarthritis, avascular necrosis, and atypical avascular necrosis, these combs become occluded (blocked) with calcium, obstructing blood flow through the bone. As the amount of occluded marrow spaces increases, the excess fat has fewer places to go, the pressure within the bone increases, and the fat attempts to escape the bone at the bone’s weakest point, the osteochondral junction. In doing so, an osteophyte is created.
The doctor may see calcifications within the bone on x-ray and call it sclerosis (dense and hard bone) or avascular necrosis, depending on the location of the calcifications. The cartilage overlying the sclerotic bone thins, and over time, the joint space narrows (bone on bone). More importantly, the oxLDL may be released into the joint through developing osteophytes. The oxLDL contributes to the destruction of the cartilage by causing cartilage cell death8 and cartilage cell senescence (age-related degeneration) may contribute to the destruction of the joint as well.9 The oxLDL also causes inflammation of the joint. The disease continues as increasing amounts of fat are ingested and deposited in the bone. This is not to say that fat is the sole cause of osteoarthritis--fat and oxLDL play a role in the initiation and progression of disease. The osteophytes, as they form, may trap the menisci and other structures in the knee leading to abnormal motion of the joint, which accelerates the wear of the cartilage. The above was not recognized by Moseley and Kirkley. Thus, the findings in their papers that arthroscopy is ineffective are not surprising.
Figure 1 Video Link: The video shows a small globule of fat traveling within a small blood vessel. Focus on the top left of the image. You are viewing the inside of bone and the honeycomb appearance is created by the marrow spaces. Note the small blood vessels traveling within the marrow space. The fat within the small blood vessels demonstrates how the blood flow to the bone may be obstructed. The green color is due to special imaging techniques to make the blood vessels more visible.
Figure 1 Video Link: Click Here and focus on the top left of the video at the 11 o’clock position at 3 to 4 seconds into the video.
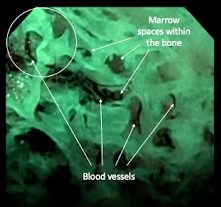
Figure 1. Click on link and focus on the blood vessel in the top left of this image to see fat traveling through the blood vessel.
Surgical Risks During an IA Saucerization
As with any surgery, an IA Saucerization has serious risks, which include, but are not limited to, pain, infection, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis [blood clots in the legs]), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus [loss of intestinal digestive movement]), vascular disorders (including thrombus [blood clots], blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including blood emboli and fat emboli, stroke or pneumonia), heart attack, and death. No implant is used for an IA Saucerization of the knee. In simple terms, when performing an IA Saucerization, the doctor must clean the knee joint thoroughly, use proper equipment and surgical technique, release intraosseous fat, and inject bone and bone marrow into the bone in the areas of excess fat and bone marrow edema lesions. If this commitment cannot be made, the procedure should not be attempted.
An IA Saucerization is NOT Routine Arthroscopy with a Different Name
An IA Saucerization is an arthroscopic procedure, but it is NOT routine arthroscopy with a different name. An IA Sauerization is a comprehensive approach to arthroscopy performed on the knee using specialized equipment in patients with osteoarthritis and a meniscus tear or other mechanical symptoms. To achieve a more thorough cleaning of the knee, better equipment is required during arthroscopy. The IA Saucerization includes: removal of all osteophytes to the extent possible, ensuring proper motion of the menisci, meniscus debridement or repair, chondroplasty, release of excess fat from the femur, reshaping of the femoral condyles and tibia as may be required, percutaneous bone grafting (not bone marrow aspiration) from the hip, super concentrating of the bone graft and bone marrow followed by its percutaneous injection into the bone in the areas where the fat is removed and bone marrow edema lesions are located. Bone grafting at the hip is achieved through a 2 mm incision when OSI’s specialized equipment is used. This is NOT simple bone marrow aspiration followed by “centrifugation” to concentrate the bone marrow aspirate. OSI’s specialized equipment eliminates the need for centrifugation because the bone and bone marrow are auto-concentrated. An IA Saucerization cannot be performed with standard arthroscopic equipment. Attempting to perform an IA Saucerization with standard arthroscopy equipment will exacerbate the patient’s symptoms. The surgeon must commit to cleaning your knee thoroughly and using the proper arthroscopic portals and equipment for the procedure. Standard arthroscopic portals were not developed for an IA Saucerization. Further, only when a non-digital 3D image is created during surgery with the OSI Clear Cannula and Q Arthroscope can the full-dimensional anatomy of the bone spurs be appreciated. This spatial orientation is critical in providing the surgeon with a dynamic understanding of how your knee functions and how your pain develops while using your knee. This information, combined with proper technique and equipment, contributes significantly to a good outcome. Individual results may vary, and a knee replacement may ultimately be medically necessary. Talk to your doctor about whether an IA Saucerization is right for you.
Consider the Facts
The IA Saucerization aims to eliminate your pain, improve the function of your natural knee, and improve the health of your bones. You and your doctor must work together as a team with the shared goal of preserving your joint. When an IA Saucerization is properly performed on a patient committed to reducing their fat intake and following the doctor’s postoperative instructions, a good outcome is more likely. Ask yourself, “What can my doctor and I do together as a team to preserve my joint?” Before and after the procedure, you must consider that your knee is worth saving. Therefore, early recognition of disease and lifestyle and diet changes are important first steps in maintaining overall good health and keeping your natural joints.
Your doctor will counsel you about how best to maintain your activities to improve the health of your knee. Such strategies may include daily walking, jogging, running, swimming, kneeling, and other home exercises so long as your health and strength of the bone are optimal. Following your doctor’s instructions regarding post-surgery activity and follow-up care is essential. However, the patient must also consider that saturated fats and trans fat contribute to osteoarthritis.
The human knee joint is a unique structure, and any problems we have require extraordinary care similar to that of a parent with a BandAid or that of a caring orthopaedic surgeon during the latter years of our life. Ask your doctor if an Intraarticular Saucerization is right for you.
References
- Moseley JB, et al. A Controlled Trial of Arthroscopic Surgery for Osteoarthritis of the Knee. N Engl J Med 2002; 34:81-88. DOI: 10.1056/NEJMoa013259. This paper concludes that arthroscopy for osteoarthritis is ineffective. However, these authors describe inadequate debridement of the knee, in our view. Further, no description of meniscus function nor the release of the excess fat from the bone is described after debridement. The meniscus appears to have been removed in some cases. The paper describes the procedure as below:
“After diagnostic arthroscopy in patients in the débridement group, the joint was lavaged with at least 10 liters of fluid, rough articular cartilage was shaved (chondroplasty was performed), loose debris was removed, all torn or degenerated meniscal fragments were trimmed, and the remaining meniscus was smoothed to a firm and stable rim. No abrasion arthroplasty or microfracture was performed. Typically, bone spurs were not removed, but any spurs from the tibial spine area that blocked full extension were shaved smooth.”
- Kirkley A, et al. A Randomized Trial of Arthroscopic Surgery for Osteoarthritis of the Knee. N Engl J Med 2008; 359:109-110. DOI: 10.1056/NEJMoa0708333.
This paper is a follow-up to the Moseley, et al. paper after the orthopaedic community considered its statistical methods inadequate. Nonetheless, Kirkley, et al. concluded that arthroscopy for osteoarthritis was ineffective after performing what appears to be inadequate debridement using antiquated equipment, as in the Moseley paper. The paper describes the procedure as below:
“Arthroscopic treatment was performed within 6 weeks after randomization with the patient under general anesthesia and with the use of a tourniquet and a thigh holder. The orthopedic surgeon evaluated the medial, lateral, and patellofemoral joint compartments, graded articular lesions according to the Outerbridge classification, irrigated the compartment with at least 1 liter of saline, and performed one or more of the following treatments: synovectomy; débridement; or excision of degenerative tears of the menisci, fragments of articular cartilage, or chondral flaps and osteophytes that prevented full extension. Abrasion or microfracture of chondral defects was not performed.”
- Ma JN, Li XL, Liang P, et al. When can total knee arthroplasty be safely performed following prior arthroscopy?. BMC Musculoskelet Disord 22, 2 (2021) https://doi.org/10.1186/s12891-020-03859-1.
- American Academy of Orthopaedic Surgeons Management of Osteoarthritis of the Knee (Non-Arthroplasty) Evidence-Based Clinical Practice Guideline (3rd Edition) https://www.aaos.org/oak3cpg, Published August 31, 2021.
- Brannon JK. Nontraumatic osteonecrosis of the femoral head: endoscopic visualization of its avascular burden. Orthopedics. 2012 Sep;35(9):e1314-22. DOI: 10.3928/01477447-20120822-15. PMID: 22955395.
- Freund E. BILATERAL ASEPTIC NECROSIS OF THE FEMORAL HEAD: PROBLEMS ARISING IN A COMPENSATION CASE. Ann Surg. 1936;104(1):100-106. DOI:10.1097/ 00000658-193607000-00010.
- Boraiah S, Dyke JP, Hettrich C, Parker RJ, Miller A, Helfet D, Lorich D. Assessment of vascularity of the femoral head using gadolinium (Gd-DTPA)-enhanced magnetic resonance imaging. A CADAVER STUDY https://doi.org/10.1302/0301-620X.91B1.2175.
- Hashimoto K, Akagi M. The role of oxidation of low-density lipids in pathogenesis of osteoarthritis: A narrative review. J Int Med Res. 2020;48(6):300060520931609. DOI:10.1177/0300060520931609.
- Martin JA, Buckwalter JA. Roles of articular cartilage aging and chondrocyte senescence in the pathogenesis of osteoarthritis. Iowa Orthop J. 2001;21:1-7. PMID: 11813939; PMCID: PMC1888191.