Please review our Terms of Use before proceeding. OSI wishes to repeat and make clear that by reviewing the following, either on a digital screen or in printed format, you (or any reviewer hereof) acknowledge, without exception, that you (or any reviewer hereof) have/has reviewed OSI’s Terms of Use. The information below is not in simple bullet points and represents nothing more than information. Joint preservation cannot be described in one or two structured sentences and simple bullet points. A broader understanding of osteoarthritis is required for a committed surgeon to perform a successful Intraarticular Saucerization. Quick and simple answers and sound bites have been avoided because patients need to be engaged in their healthcare and talk to their doctors. In this regard, a reader hereof may find the information below interesting. Indeed, one is always desirous of immediate relief from pain, and it is for this reason that any reviewer hereof must talk to their doctor. OSI encourages all of us to be informed so that we can avoid ever reaching a point wherein a joint replacement is our only option. Ask questions and be engaged.
To understand knee pain, let’s first describe how the knee bones come together to make the knee joint. The working parts of the knee joint consist of three bones: the shinbone (tibia), the thigh bone (femur), and the kneecap (patella). Where the tibia connects to the femur is called the knee joint. The ends of the femur and tibia are covered with cartilage. The patella helps keep the knee straight while walking, and its undersurface is covered with cartilage as well. The knee joint also has important bands that hold the bones together called ligaments. Additionally, the knee joint has cushioning washers between the femur and tibia called menisci. The menisci glide along with the cartilage in the knee when the knee is in motion while walking, running, kneeling, or jumping. The knee joint lining produces a lubricant called synovial fluid that helps with the gliding of the menisci along the cartilage.
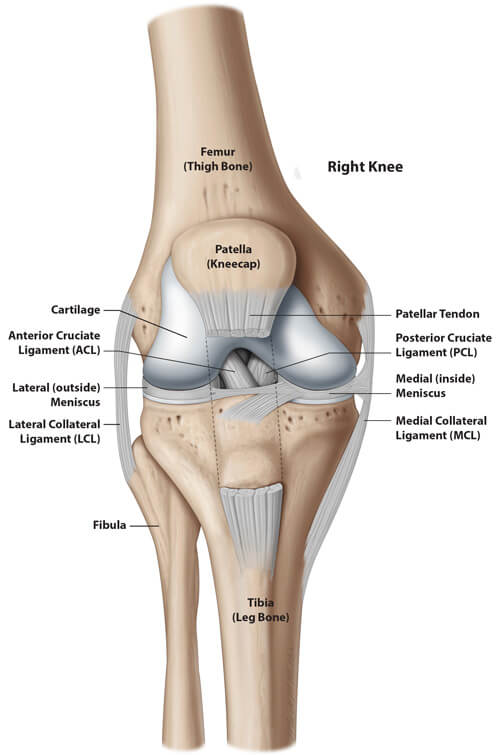
The most important function of the knee is walking. When walking, one leg is raised off of the ground causing the knee to bend while standing on the opposite leg. While the knee is bending, the menisci must glide smoothly along the cartilage toward the back of the knee. As you progress through walking, the patella will then help straighten the knee before the heel strikes the ground. While straightening the knee, it is important for the menisci to glide forward now to cushion the cartilage when the heel strikes the ground.
Knee pain results when the working parts of the knee do not operate together smoothly. Any of a number of diseases, changes in body weight, or trauma can alter how the working parts of the knee operate together. A common disease affecting the working parts of the knee in people over the age of 50 is osteoarthritis (OA). Thus, in addition to treating pain within the knee joint, treatment should also include making sure that the working parts of the knee operate together smoothly. If the treatment only masks the pain in a knee with abnormal working parts, things may worsen.
It depends on the cause. A comprehensive treatment plan for pain due to osteoarthritis of the knee, if saving the joint is desired, may range from nonsurgical reassurance with NSAIDs, such as Advil, to a minimally invasive Intraarticular (IA) Saucerization, see below. A joint replacement may be performed if the knee condition is not suitable for joint preservation. An x-ray will be taken during treatment planning, allowing the surgeon to see the knee bones and how they fit together. An MRI of the knee allows the surgeon to see the menisci, the cartilage, the ligaments, the tendons, and the insides of the bones. A knee may experience pain during certain motions, and x-rays and MRIs do not show this relationship. The x-ray and MRI are taken while the knee is not in motion. This is why it is important to explain to your surgeon the specific problem you are having with your knee and in what positions the pain worsens or is its worst.
An IA Saucerization of the knee is an advanced arthroscopy procedure using specialized arthroscopes and equipment that reshape the bones of the knee by removing bone spurs (osteophytes) in the front and back of the knee that cause abnormal contact between the knee structures while walking. The IA Saucerization is not arthroscopy of the knee with a different name. The IA Sauerization also recontours the cartilage where it is torn and ensures proper function of the meniscus by cleaning or repairing it and by removing any osteophytes that block it from gliding backward and forward while walking. This assessment is made while in surgery and never assumes that the only problem with the meniscus is the tear observed on a preoperative MRI. Osteophytes form when fat attempts to escape the bone at the bone’s weakest point, the osteochondral junction (OCJ). See Figure 2.

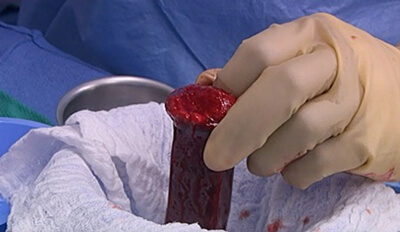
These bone spurs are easily seen on x-ray and have a characteristic shape that results from motion of the knee. During an IA Saucerization, the surgeon removes these bone spurs and others, and decompresses the thigh bone by allowing the excess fat to exit through the debrided bone spurs. Spongy (cancellous) bone and bone marrow are taken from the hip above the knee and injected into the bone to replace the excess fat, restoring the biology to the bone. Traditionally, the knee joint is simply debrided and no efforts are made to decompress the femur of its excess fat. Fat attempts to escape the bone at the bone’s weakest point, the osteochondral junction.
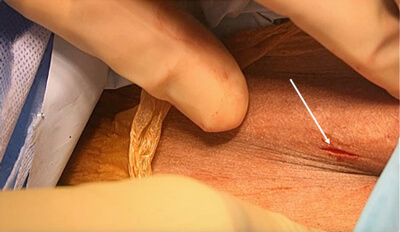
As the knee moves, the bone spurs are shaped as shown by the arrow. Additionally, oxLDL are released into the joint. The oxLDL can destroy the cartilage and cause inflammation. Figure 3A shows the autologous morselized bone obtained from the hip during an IA Saucerization. Figure 3B shows the small incisions used to harvest the bone.
The embedded video, Intravascular Fat Video, demonstrates intravascular fat within the capillary network within the bone. A reviewer hereof is asked to focus on the 11 o’clock position at 3 to 5 seconds within the video. Of the three main food substances, fat is the only substance that does NOT pass through the liver before entering the circulation and as a result it can be readily deposited in the bone and many other parts of the body.
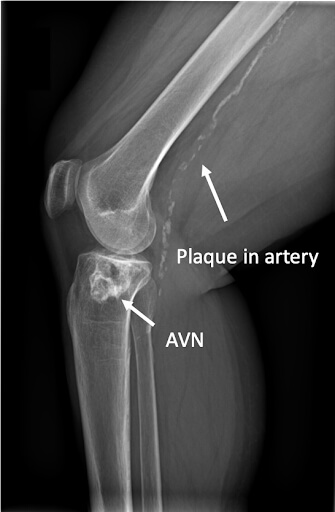
Upon reading the information provided herein, it is likely to be assumed that sufficient stem cells are present for new bone formation in an arthritic knee. Thus, concentrated PRP may be considered for injection directly into the bone of an arthritic knee to avoid taking bone graft and bone marrow from the hip in an attempt to perform an office-based procedure. Importantly, injecting any medicament into the bone without properly allowing the fat to exit could lead to fat embolization (a large globule of fat circulating in the blood). The IA Saucerization recognizes that the blood flow to localized areas of bone has been compromised for many years by the excess fat and calcification of the marrow spaces, as evidenced by the bone spurs increasing in number and size over time (mild, moderate, or severe osteoarthritis). Investigators have recently described the destruction of cartilage by oxidized low-density lipoproteins (oxLDL) but appear not to have recognized that the source of the oxLDL is the bone itself through developing bone spurs. This important connection comes from observing obstructed blood flow on intraosseous endoscopy in cases of avascular necrosis and osteoarthritis,1 occluded marrow spaces,2 and the detection of oxLDL within bone marrow edema lesions and synovial fluid in arthritic knees. A similar calcification process due to oxLDL occurs in the peripheral arteries and the arteries around the heart. See Figure 4.
OxLDL has been shown to disrupt the normal function of bone-forming cells, osteoblast, and osteoclast.3,4,5 The IA Saucerization recognizes that the cartilage and bone are not healthy in the case of osteoarthritis and at a minimum, the quality of the bone should be assessed if considering arthroscopy for osteoarthritis with a meniscus tear.
The cancellous bone and bone marrow injected directly into the bone improve the bone’s health and strength. An IA Saucerization should not be performed using traditional arthroscopes.6,7 Traditional arthroscopes are too short and too large and do not have the water flow properties necessary for a successful IA Saucerization.
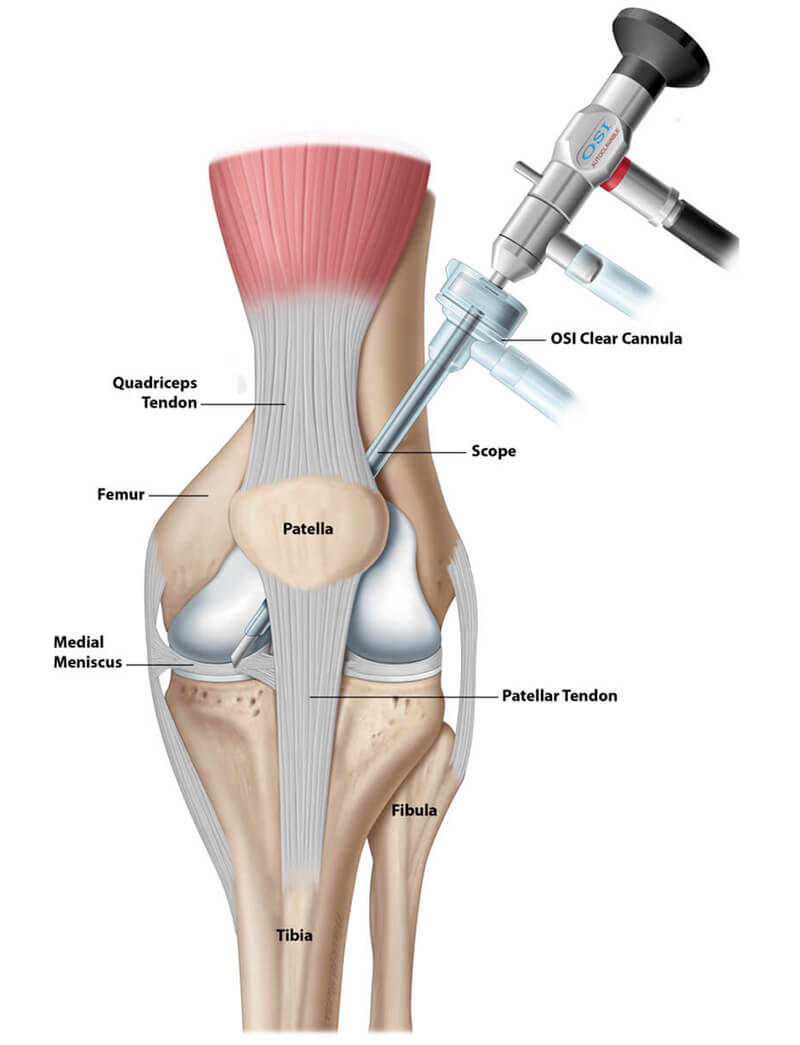
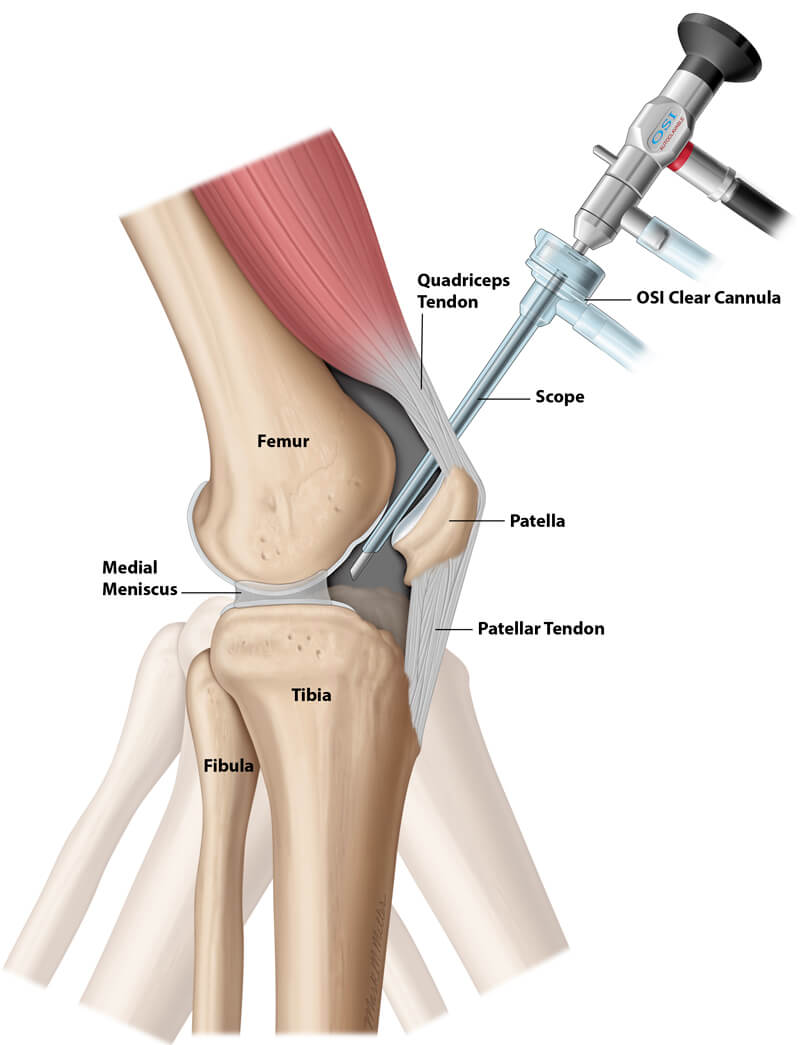
The skilled surgeon performs the IA Saucerization through two to three small incisions while repeatedly motioning the knee as if the patient were walking. Fluoroscopy may be used as well. On the morning of surgery, the patient is asked to mark the most painful areas of the knee. This helps the surgeon to focus immediately on these areas during surgery. The blood pressure and heart rate are monitored for changes indicating that the areas being cleaned and reshaped are likely the source of the pain. These painful areas are matched to the ink markings placed on the skin by the patient. The surgeon correlates the arthroscopic findings with the patient’s history, physical examination, x-rays, and MRI and ensures that the anatomy of the knee is restored to as near normal as possible and that the menisci are moving backward and forward rather smoothly after being cleaned or repaired. See Figure 5 and Figure 6.
An IA Saucerization can be performed with or without a tourniquet. Your doctor may require you to use crutches for 2 to 4 weeks after surgery, and home exercises may be used as physical therapy. A continuous passive motion machine (CPM), as may be the case after a total knee, is not required. Given the very small incisions, significant scarring after surgery is unlikely. Most patients can go home the day of surgery.
The IA Saucerization considers the limitations of x-rays and MRIs to show the abnormal motion relationships between the working parts of the knee and how this abnormal motion brings on pain and deformity. For example, the images of x-rays and MRIs do not show how a bone spur on the tibia strikes the front of the femur and causes pain when the patient stands from a sitting position. Therefore, to perform an IA Saucerization of the knee, specialized equipment must be used, and the surgeon must place the arthroscopic instruments into the joint in a manner that allows the entire knee to be observed while in motion. As noted above, if it is concluded that an IA Saucerization is nothing more than routine arthroscopy with a different name and it can be achieved with current arthroscopy equipment and a standard approach, a good outcome is not likely to be realized and should be avoided. Attempting to perform an IA Saucerization with traditional equipment will exacerbate the patient’s knee pain. If the physician and hospital, where the procedure is to be performed, cannot commit to obtaining the proper equipment, the procedure should NOT be attempted. The physician performing the procedure must have a broadened understanding of osteoarthritis as noted in the peer-reviewed published literature, and be prepared to remove all accessible bone spurs to decompress the femur of excess fat. Injecting spin-downs (concentrated bone marrow aspirates or PRP from a peripheral blood draw) without removing the excess fat or irrigating the host bed of bone should be avoided. See Figure 7.
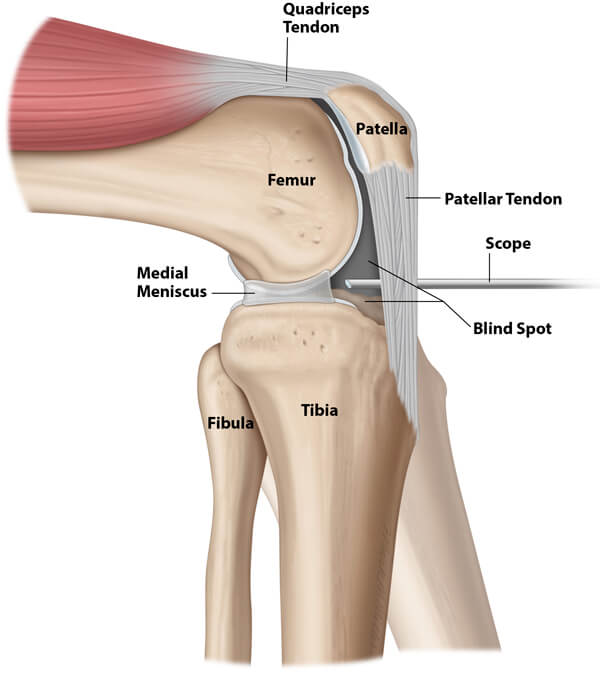
Figure 7 shows how a blind spot is created behind the lens of the arthroscope and how the position of the arthroscope will limit the raising and lowering of the leg during surgery when compared to Figures 5 and 6. Figure 7 also shows how a meniscus tear can be easily debrided or repaired (typical arthroscopy for osteoarthritis with a meniscus tear); however, the backward and forward motion of the meniscus while walking cannot be assessed because the arthroscope must move as the tibia moves.
The following questions should be considered by those interested in understanding an IA Saucerization (careful reading is required):
The presence of fat within the bone is normal, but the bone may contain excess fat due to increased consumption. Blood and fat do not mix unless the fat is in the form of a protein and phospholipid called a lipoprotein. This fat circulates in the bloodstream as low density lipoproteins that contain cholesterol (LDL-Bad Cholesterol and HDL-Good Cholesterol), but fat within the bone is stored in fat cells. Excess fat within the bone may block the inflow of blood into the bone, causing areas of localized hypoxia (low oxygen). These areas of micro hypoxia, in this sense, may be considered osteobiologic cul-de-sacs. See Figures 8A and 8B.
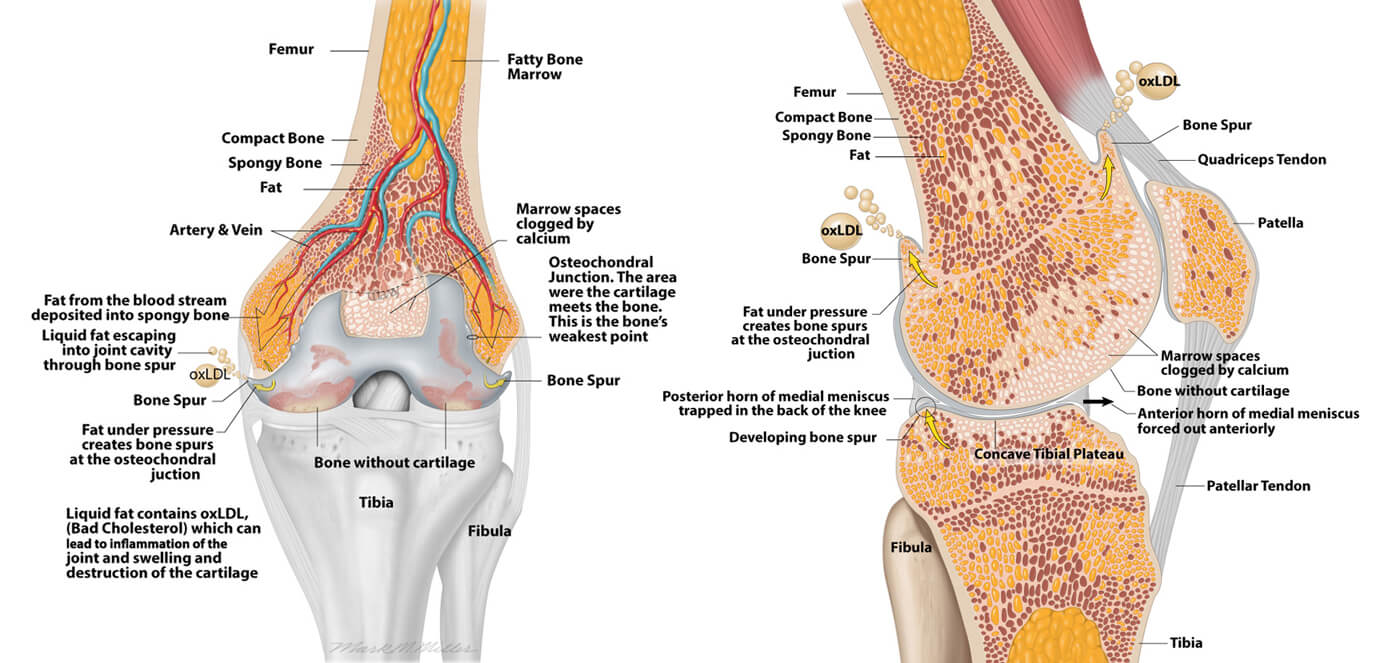
The only exit for fat once it enters the bone is through consumption as an energy source in the formation of the formed elements of blood or its release into the circulation in the case of extreme metabolic needs. Therefore, excess fat within the bone may harm the ability of blood to flow continuously into and out of the bone. As blood tries to flow into the bone, the pressure within the bone builds causing pain, and the excess fat is forced to find an exit. The excess fat will attempt to exit the bone at the bone’s weakest point (the osteochondral junction), e.g., the point where the cartilage meets the bone. As the fat attempts to exit the bone at this weak point, a balloon-type structure is created, which can be called an immature bone spur. See Figures 9A and 9B.
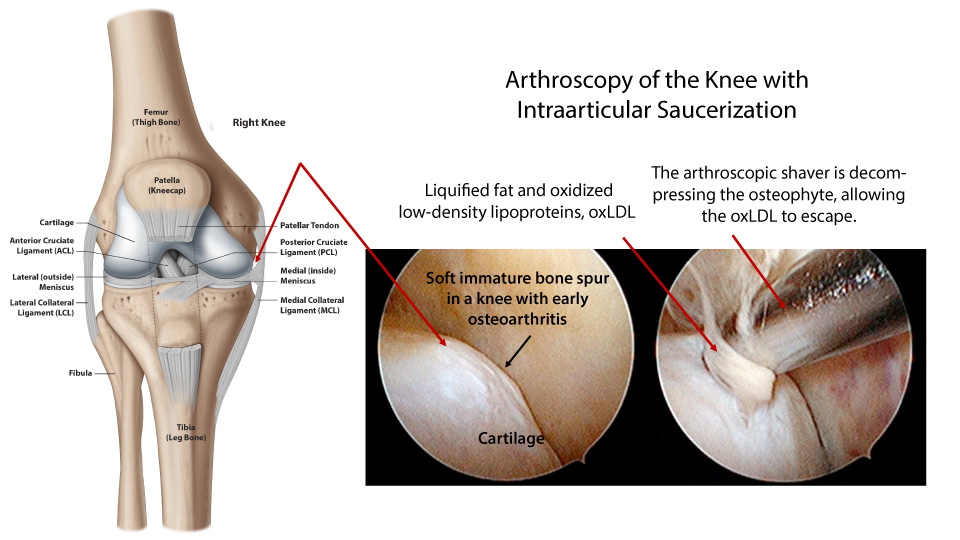
Immature bone spurs are soft and particularly painful bulges at the osteochondral junction because the bone underneath the spur is weak and fractured (intraosseous insufficiency fractures). These immature bone spurs are not visible on x-ray. However, once they enlarge and mature into hard bone spurs, as shown in Figure 9B, they will appear on x-ray. The years required for these immature bone spurs to enlarge and mature into hard visible bone spurs are often the many years the patient experiences knee pain and joint swelling. This time period is called the run-up to a total knee. The motion of the knee joint further shapes these bone spurs or causes them to break off, leading to having a loose body within the joint. Loose bodies may also be fragments of cartilage. Thinning of the cartilage and deformity is also a part of the disease. Thinning of the cartilage is due to sclerosis (calcification of marrow spaces) of the underlying bone and destruction of the cartilage by oxLDLs and senescence (deterioration with age) of chondrocytes (cartilage cells).3,4,5,8,9,10 Bone marrow edema may develop in localized areas of excess fat and oxLDLs due to the pro-inflammatory nature of oxLDLs or result from intraosseous insufficiency fractures. These bone marrow edema lesions can be detected on MRI. As the disease progresses and the bone spurs enlarge, the menisci may become increasingly trapped and torn. X-rays will be obtained, and the patient may be advised that their osteoarthritis is mild, moderate, or severe. If the patient is selected for arthroscopy, how and why these bone spurs develop are usually not considered, nor are the bone spurs entirely removed to ensure proper function and gliding of the meniscus.5,6 Further, there is no effort to decompress the bone of the oxLDLs. This may lead to disagreement amongst surgeons about the effectiveness of arthroscopy for mild or moderate forms of osteoarthritis, and many surgeons are inclined to conclude arthroscopy is ineffective even in the face of inadequate instrumentation and inadequate debridement as described in the literature.5,6 Proper functioning of the meniscus goes beyond its repair and must include reshaping of the cartilage along the femur and the tibia, removal of obstructing bone spurs, and an evaluation of the effectiveness of these techniques in restoring proper meniscus function during surgery. A good clinical outcome is related to recognizing and treating the causative factors for the degeneration of the joint and the meniscus tear, while a good hospital outcome is achieving the above by performing reimbursable procedures at reduced costs. Again, a total joint is a good procedure when it is indicated. At OSI our focus is on preserving the joint during the run-up to a joint replacement by developing products that address the underlying cause of osteoarthritis as we understand it. Our understanding is well-supported in the peer-reviewed published literature. That said, the surgeon must use the proper tools and the surgical approach to achieve the above goals. Traditional arthroscopic tools are not effective for arthroscopy of a knee with osteoarthritis. Non-digital 3D images can not be obtained with traditional arthroscopes. Currently available arthroscopes were developed in the 70s. When an Intraarticular Saucerization is performed using OSI’s specialized equipment, bone spurs are unroofed and removed in the front and back of the knee where accessible. The excess fat and oxLDLs can then exit the bone. More importantly, the bone is infused with an autologous bone graft slurry and bone marrow, not simply concentrated bone marrow or PRP, to improve the bone’s health by restoring its biology, replacing the excess fat with living bone and bone-forming cells. Orthopedic Sciences’ specialized tools achieve all of the above and automatically concentrates the autologous bone and bone marrow obtained from the hip. Therefore, passing a bone marrow aspirate out of the sterile field for centrifugation is not required, as this introduces the need for more OR personnel and the potential of specimen contamination.
When not considering the above during arthroscopy for degenerative arthritis with a meniscus tear, good outcomes are less likely, and continued non-operative measures such as NSAIDs (Advil), PT, injections, viscosupplements, and opioids in some cases, potentially move patients with knee pain to an inevitable replacement. This kind of care is delivered against a background of diminishing enthusiasm and reimbursement amongst providers (burnout) and an ever increasing number of revisions.
The patient and physician are encouraged to recognize how the American diet contributes to osteoarthritis as it does to coronary artery disease, diabetes, peripheral vascular disease, hypertension, and stroke. For this reason, it is important for the patient to make dietary changes as a contribution to preserving their natural joints. The Intraarticular Saucerization is the first and only procedure that combines a comprehensive view of joint disease, supported by published literature, into a single minimally invasive procedure for joint preservation. OSI does not produce products as bandaids nor products to replace joints. We encourage patients to talk to their doctors about their knee pain early in the disease process and to discuss further how the American diet contributes to disease. We encourage physicians to think deeply about the causes of bone spur formation, oxLDLs, and the mechanics of the arthritic joint beyond varus or valgus malalignment and patella tracking. All of the patented technology at OSI was developed with the above in mind. Many patients that have had a saucerization have been able to keep the joint they were born with for more than 16 years!
Joint replacement of the knee is a cleaning of the knee that is so extensive an artificial joint must be inserted in the place of the normal knee joint. A knee replacement is not a resurfacing procedure. The name resurfacing implies that a loss of cartilage is the primary problem and the bone beneath the cartilage is healthy. Labeling a total knee as a resurfacing procedure is nothing more than using a sound bite to describe a poorly understood disease. In osteoarthritis, the cartilage and the bone are diseased. While many surgeons attempt to “preserve” bone during a replacement, bone is invariably removed. Preservation of bone in this sense is in anticipation of having sufficient bone stock if and when a revision arthroplasty is ever required.11 A successful knee replacement requires the implant to be fixed to healthy bone among many other things. The surgeon may perform the replacement in a traditional manner or use the assistance of a robot. When performing the replacement (cleaning the knee joint extensively), the cuts of the bone must follow a particular pattern so that the artificial components can be attached to the femur, the tibia, and the patella. The components may be fixed to the bone with or without cement. During a primary total knee replacement (the first time for replacement), the surgeon usually does not treat any underlying bone problem. Additionally, the procedure will attempt to correct any abnormal joint alignment if the patient has bowed legs or knocked knees.
This paper concludes that arthroscopy for osteoarthritis is ineffective. However, these authors describe inadequate debridement of the knee. Further, no description of meniscus function after debridement is described nor the release of the excess fat from the bone. The meniscus appears to have been removed in some cases. The paper describes the procedure as follows:
“After diagnostic arthroscopy in patients in the débridement group, the joint was lavaged with at least 10 liters of fluid, rough articular cartilage was shaved (chondroplasty was performed), loose debris was removed, all torn or degenerated meniscal fragments were trimmed, and the remaining meniscus was smoothed to a firm and stable rim. No abrasion arthroplasty or microfracture was performed. Typically, bone spurs were not removed, but any spurs from the tibial spine area that blocked full extension were shaved smooth.”
This paper is a follow-up to the Moseley, et al. paper after the orthopaedic community considered its statistical methods inadequate. Nonetheless, Kirkley, et al. concluded that arthroscopy for osteoarthritis was ineffective after unwittingly performing inadequate debridement and using antiquated equipment, as in the Moseley paper. The paper describes the procedure as follows:
“Arthroscopic treatment was performed within 6 weeks after randomization with the patient under general anesthesia and with the use of a tourniquet and a thigh holder. The orthopedic surgeon evaluated the medial, lateral, and patellofemoral joint compartments, graded articular lesions according to the Outerbridge classification, irrigated the compartment with at least 1 liter of saline, and performed one or more of the following treatments: synovectomy; débridement; or excision of degenerative tears of the menisci, fragments of articular cartilage, or chondral flaps and osteophytes that prevented full extension. Abrasion or microfracture of chondral defects was not performed.”
Klug A, Gramlich Y, Rudert M, Drees P, Hoffmann R, Weißenberger M, Kutzner KP. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc. 2021 Oct;29(10):3287-3298. DOI: 10.1007/s00167-020-06154-7. Epub 2020 Jul 15. PMID: 32671435; PMCID: PMC7362328.